Depression and lifestyle: 13 golden tips
Source: Jeleefstijlalsmedicijn
More and more research shows that lifestyle plays a crucial role
in depression. Nutrition, exercise, sleep, relaxation, and even meaning
influence not only how we feel but also how our brains and
metabolism function. In this article, we dive deep into the relationship
between depression and metabolic dysfunction, and we show how
lifestyle interventions can help improve mood and energy.
Do you want to know which lifestyle factors really make a difference and how to
apply lifestyle measures in practice? Read on and discover how
you — or someone around you — can take the first step toward recovery.
Reading time 15 minutes
Author: Jaap Versfelt
Medical-scientific reviewer: prof. dr. Rogier Hoenders, psychiatrist
and professor of spirituality, lifestyle, and mental health at the
University of Groningen
Key points from this article:
Section titled “Key points from this article:”- What is depression?
Depression is a common mental disorder with symptoms such as persistent sad mood, fatigue, and loss of pleasure. - How common is depression and is it growing?
About a quarter of adults in the Netherlands will experience depression at some point. The percentage of depressed adults has almost doubled over the past 15 years. - Metabolic dysfunction as a risk factor for depression
Metabolic dysfunction, characterized by overweight, high blood pressure, and disrupted blood sugar levels, is more common in people with depression. - Limitations of current treatment methods
Psychotherapy and medication are not always effective and often have side effects. Antidepressants can lead to weight gain, sexual dysfunction, and metabolic syndrome. - Lifestyle interventions as a complement to depression treatment
Lifestyle changes can help with depressive symptoms and improve metabolic health. - Healthy nutrition
Ultra-processed food increases the risk of depression. A Mediterranean diet, rich in vegetables, fruit, fish, and olive oil, can potentially reduce depressive symptoms. - Regular exercise
Exercise such as walking, jogging, and yoga is as effective as cognitive behavioral therapy and for mild to moderate depression possibly even more effective than antidepressants, with positive rather than negative side effects. - Good sleep
90 percent of people with depression have sleep problems; the relationship is complex. Treatments can be aimed at both increasing the duration and quality of sleep, but sometimes also at sleep restriction. - Relaxation and stress reduction
Chronic stress increases the risk of depression. Techniques such as breathing exercises and mindfulness help with relaxation. - Substance use
Alcohol and drug use are more common in people with depression and can reduce the effectiveness of treatments. - Meaning
A strong sense of meaning is linked to better mental health and fewer depressive symptoms. - How do you achieve lifestyle change?
Thirteen strategies, such as setting achievable goals, tracking successes, and following role models, help maintain a healthy lifestyle. - Conclusion
Lifestyle change can play an important role in the treatment and prevention of depression and metabolic conditions.
1. What is depression?
Section titled “1. What is depression?”Depression is one of the most common mental disorders in the world and is characterized by a persistent sad mood, loss of interests or pleasure, fatigue, and often also physical complaints. According to the DSM-5 (the diagnostic manual for mental disorders), symptoms such as concentration problems, feelings of worthlessness, changes in appetite and sleep patterns, and even suicidal thoughts can be part of the clinical picture. It is important to understand that depression is more than a feeling of sadness. It is a complex condition with biological, psychological, and social dimensions.
2. How common is depression and is it growing?
Section titled “2. How common is depression and is it growing?”In the Netherlands, about a quarter of adults will experience depression at some point in their lives. Each year, this applies to about 9 percent of adults. Women in the age category 18-34 years have the highest chance of depression (Trimbos, 2022). In 2007-2009, 5.1 percent of adults in the Netherlands had a depressive disorder. By 2019-2022, this had almost doubled to 9.3 percent (VzInfo, 2022).
3. Metabolic dysfunction as a risk factor for depression
Section titled “3. Metabolic dysfunction as a risk factor for depression”Depression is caused by a combination of physical, psychological, and social factors. Among the physical factors, metabolic dysfunction plays a major role.
3.1 Metabolic dysfunction is associated with depression
Section titled “3.1 Metabolic dysfunction is associated with depression”The physical condition of patients with a serious mental disorder is often not strong. Compared to the general population, their chance of death is two to three times greater. As a result, they live on average 10 to 20 years shorter, mainly due to cardiovascular disease (Deenik, 2019).
A major role here is played by metabolic syndrome. In people with metabolic syndrome, metabolism is dysregulated. The syndrome is also characterized by a large waist circumference, elevated blood pressure, elevated blood sugar levels, and abnormal cholesterol values.
Metabolic dysfunction increases the chance of type 2 diabetes, cardiovascular disease (Yusuf, 2004), and many other chronic diseases. Metabolic dysfunction is more common in people with depression than in the general population (Vancampfort, 2015).
Metabolic dysfunction is caused, among other things, by unhealthy lifestyle influences such as eating ultra-processed food, insufficient exercise, lack of sleep, and stress.
3.2 Metabolic dysfunction and depression: chicken or egg?
Section titled “3.2 Metabolic dysfunction and depression: chicken or egg?”We know that metabolic dysfunction and depression are related. But in what way are they related? Research shows that they reinforce each other (Semenkovich, 2015):
- Depression increases the chance of metabolic dysfunction. People with severe depression have a two times greater risk of developing the metabolic condition type 2 diabetes (Eaton, 1996). Additionally, researchers observe worsened metabolism during depressive episodes of patients. This worsened metabolism recovered after six months of treatment with antidepressants (Tayeb, 2023).
- Metabolic conditions increase the chance of depression. Research shows that patients with type 2 diabetes have a 24 percent higher risk of depression (Nouwen, 2010). Addressing insulin resistance (a precursor to type 2 diabetes) in the treatment of depression leads to faster recovery and prevention of relapse (Watson, 2018).
Metabolic dysfunction can be addressed with lifestyle change. Certain lifestyle changes appear to have a positive effect on people with depression (we will see this in chapter 6). This is good news for people with depression, because the current treatment of depression, however valuable, has limitations.
4. Limitations of current treatment methods for depression
Section titled “4. Limitations of current treatment methods for depression”The current treatment methods in mental health care, including psychotherapy and medication, have undeniable value. However, there are limitations in terms of effectiveness, and there are often bothersome side effects.
- Limited effectiveness Although psychopharmaceuticals and psychotherapy can be effective treatment options, they do not always lead to complete remission. For example, less than half (46 percent) of patients who receive medication achieve remission where symptoms largely or completely disappear (Casacelanda, 2002).
- Side effects and tapering Medication can have significant side effects. Antipsychotics can lead to weight gain and metabolic syndrome, and increase the chance of type 2 diabetes. Additionally, antidepressants often cause side effects such as sexual dysfunction, weight gain, and insomnia. There are also sometimes significant withdrawal symptoms.
- Medicalization Mental conditions are increasingly being diagnosed and treated with medication, but there is a growing discussion about the risk of medicalizing normal variation in human experiences. A little restlessness is sometimes too quickly called ADHD, and feelings of sadness and grief are sometimes too quickly classified as depression (Dehue, 2023).
- Not treating physical conditions In our healthcare system, physical and mental care are offered separately. This is sometimes problematic because psychiatric patients often have physical conditions such as cardiovascular disease and type 2 diabetes (Schillemans, 2024). Moreover, people with these physical conditions more often have depressive complaints. Patients with diabetes, for example, have a two times greater risk of depression (Semenkovich, 2015).
5. How lifestyle interventions can help reduce depressive symptoms
Section titled “5. How lifestyle interventions can help reduce depressive symptoms”The good news is that metabolic dysfunction can be improved with lifestyle interventions. With better nutrition, more exercise, better sleep, relaxation, stopping substance use, and through meaning, people can not only improve their physical health but possibly also counter their depressive symptoms.
5.1 Healthy nutrition
Section titled “5.1 Healthy nutrition”A diet rich in ultra-processed foods and lots of sugar
increases the risk of depression (Samuthpongtorn,
2023). Ultra-processed products are, for example,
soft drinks, chips, cookies, candy, ready-made meals, and fast food.
We eat a lot of such food: 61 percent of the calories of the
average Dutch person comes from ultra-processed food (even 75 percent
for children) (Vellinga,
2022).
A different dietary pattern can help. The Mediterranean diet is an
example of this, as a randomized study (the ‘Smiles Trial’) shows.
The diet includes vegetables, fruit, nuts, olive oil, fish, and
whole grains, a limited intake of alcohol and dairy, and it has
a small intake of red or processed meat and sweet snacks. Eating this
way leads to major improvements in mood in people with
depression. 32 percent of participants in the study even achieved
complete remission (Jacka,
2017). It should be noted that
criticism was raised about the design of the study. Replication of the study is
needed to strengthen the evidence.
In addition to the Mediterranean diet, there are other diets that may possibly help with depression. Recently, there has been much attention to the effect of the ketogenic diet on brain disorders (such as epilepsy and autism). However, there are no randomized studies yet that demonstrate the effectiveness of the diet in people with depression. There are case reports that show that some people have success with it (such as Calabrese, 2024).
5.2 Regular exercise
Section titled “5.2 Regular exercise”Patients with a serious mental disorder spend on average more
time sitting or lying down than the general population (Deenik,
2018). This lack of physical activity (such as
a lot of sitting and little exercise) is a risk factor for depression
(Schuch,
2016).
An analysis of 218 studies on exercise and depression showed that
more exercise is an effective treatment for depression. Dancing,
walking, jogging, yoga, and strength training are the most
effective, especially at high intensity (Noetel,
2024).
Interestingly, the effect of exercise:
- Is comparable to the effect of cognitive behavioral therapy.
- Is possibly even greater than that of antidepressants such as SSRIs
(selective serotonin reuptake inhibitors), a commonly used group of
medications for depression, for mild or moderate depression.
See figure 1 for the effect size of exercise versus these ‘traditional’ forms of treatment.
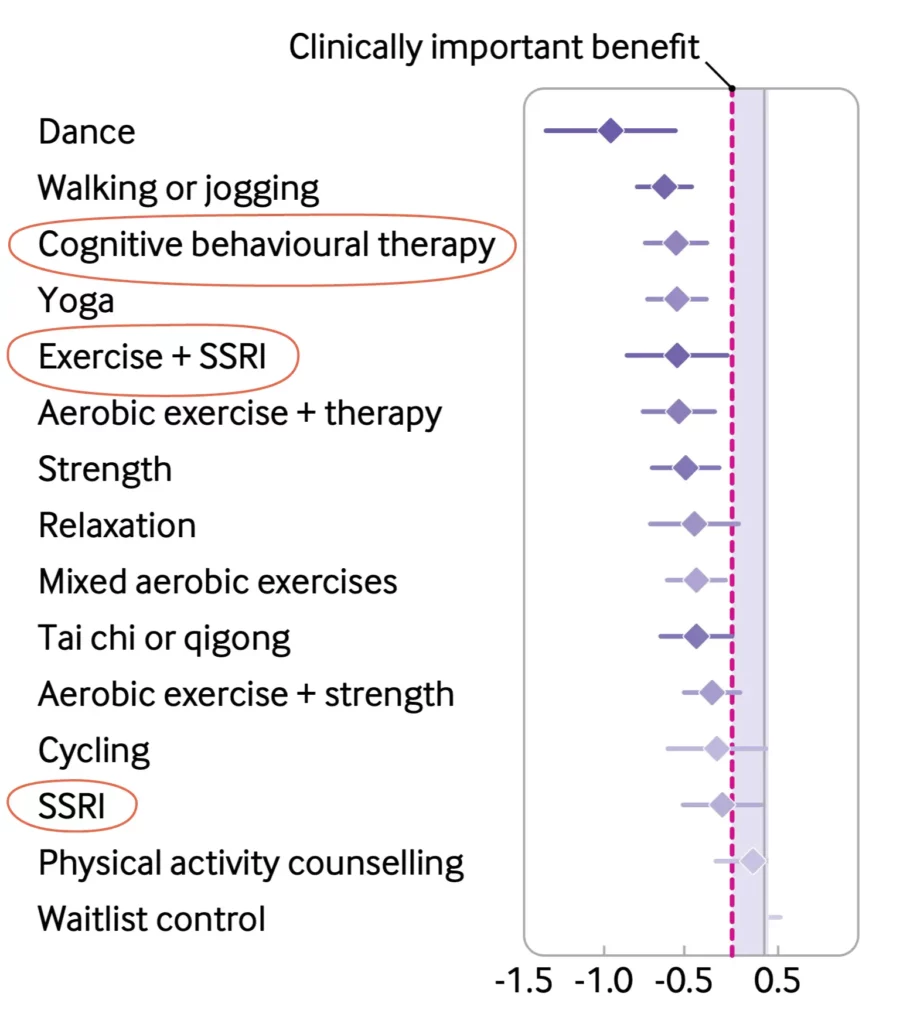
Figure 1: effect of exercise on symptoms of depression (Noetel, 2024)
5.3 Good sleep
Section titled “5.3 Good sleep”90 percent of people with depression have sleep problems (Soehner,
2014).
The relationship between sleep and depression is complex; in depression, both
an increase and decrease in sleep is reported, and in treatment,
sometimes the focus is on more sleep and sometimes on less sleep
(sleep deprivation) (Bouwmans,
2017).
5.4 Relaxation
Section titled “5.4 Relaxation”Stress can increase the risk of depression by overloading
the stress system, disrupting brain areas that regulate emotions and safety
(McEwen,
2007).
It is important to reduce stress not only for general
health but certainly also for people with depression. Stress can
be a trigger for mental complaints. Reducing stress can
be done with regular relaxation, breathing exercises,
sufficient sleep, progressive muscle relaxation (where muscle groups in
the body are tensed and then relaxed), and mindfulness
based stress reduction.
5.5 Stopping substances
Section titled “5.5 Stopping substances”The use of alcohol, tobacco, or drugs is more common in people with
depression (Scott,
2011).
Excessive alcohol use, for example, can lead to depressive symptoms that
do not respond well to antidepressant medication and can reduce the
effectiveness of other treatments. Drug use, particularly
cannabis use, also increases the risk of mental
conditions such as psychoses. Therefore, it is important to not only
focus on the treatment of depression but also on reducing or
stopping substance use.
5.6 Meaning
Section titled “5.6 Meaning”People with depression often struggle with the question: ‘What is the meaning of my
life?’ The lack of meaning can reinforce feelings of hopelessness
and hinder recovery. Research shows that a strong
sense of meaning is associated with better mental health
and a smaller risk of depression.
Scientific research among the general population shows that
meaning is correlated with longer life, better health, and a
higher quality of life. This effect of meaning also exists for
mental conditions. Research shows that religious and spiritual
involvement is associated with less depression, anxiety, suicide attempts,
and addiction and faster recovery from depressive symptoms (Bonelli,
2013).
Other research shows that meaning can reduce depressive symptoms,
probably through social support and healthier
lifestyle choices (Braam,
2019).
Improving meaning can thus be a valuable addition to
depression treatments. This can be achieved, among other things, by
helping people find meaningful goals, strengthen social connections,
and actively participate in meaningful activities
(Hoenders,
2020).
Lifestyle intervention for depression — more effective and also
cheaper?
A recent pilot study (Schillemans and Hoenders,
2024) examined the effect of a
lifestyle intervention in people with serious mental conditions,
including depression. The experiment included eleven group sessions with
attention to exercise, nutrition, relaxation, sleep, substance use, and
meaning. Effects were found in all recovery areas, with
the largest effects in social recovery and the smallest in clinical
recovery. The control group received usual care, such as therapy and
medication.
Recently, a second, larger, controlled pilot study was done with
an adapted version of the first pilot. Again, positive
effects were found. The cost-effectiveness analysis of the second
pilot showed that total societal costs over 21 weeks
were lower in the experimental group (EUR 5,052) than in the control group
(EUR 7,452). The savings came mainly from lower costs for
sheltered housing, psychotherapy, and social services.
The research provides additional evidence for the potential of
lifestyle adjustments as a valuable addition to regular
treatments for depression, both in terms of effectiveness and
costs.
6. The relationship between metabolic dysfunction and depression
Section titled “6. The relationship between metabolic dysfunction and depression”How is it possible that something as basic as a healthy lifestyle can prevent mental disorders, or even restore them to some extent? To explain this, some physiological mechanisms have been proposed in science (Swainson, 2023).
6.1 Dysregulation of the stress axis
Section titled “6.1 Dysregulation of the stress axis”The hypothalamic-pituitary-adrenal axis (HPA axis) regulates the stress response, but in depression, this is often dysregulated. This leads to overproduction of cortisol, which can worsen mood complaints. Prolonged stressful circumstances and unhealthy nutrition can reinforce the dysregulation (Hoenders, 2020).
6.2 Low-grade inflammation
Section titled “6.2 Low-grade inflammation”Chronic low-grade inflammation is common in metabolic dysfunction and can worsen depressive symptoms. Inflammatory substances such as C-reactive protein (CRP) and interleukin-6 are elevated by a diet with lots of processed food and sugars.
6.3 Obesity
Section titled “6.3 Obesity”Obesity increases the risk of depression. Obesity can disrupt neurotransmitters, overstimulate the HPA axis, and cause inflammation, which worsens depressive symptoms.
7. Tackling depression with lifestyle: 13 golden tips
Section titled “7. Tackling depression with lifestyle: 13 golden tips”Implementing lifestyle changes is not easy. For people with depression, the challenge can be even greater because depression often comes with symptoms such as fatigue, loss of motivation, and negative thoughts, which make behavioral changes difficult.
Yet there are ways to overcome the obstacles. Rogier Hoenders and colleagues from the Center for Integrative Psychiatry and the Lifestyle Team of Lentis (a large mental health institution in the North and Central Netherlands) work with thirteen golden tips**:**
- Find reliable and understandable lifestyle information
Not everything you read online is true. Choose sources that are clear and scientifically substantiated. - Become aware of your own behavior
Mindfulness is crucial in every phase of behavioral change. Only when you notice what you are doing can you change something. - Keep track of what you do for a week
We often have a distorted picture of ourselves and our memory is not (always) reliable. Write down for a week how you eat, exercise, and sleep. This provides insight and motivation. - Record successes
Note small changes that have succeeded, such as an extra glass of water or a walk after eating. This reinforces new behavior. - Set an achievable goal
Use the SMART-PLUS method (Specific, Measurable, Acceptable, Realistic, Time-bound AND Positive, Fun, Urgent, Individual, Easy) to set goals. This makes what you are going to do fun and manageable. - Work with small, repeatable steps (Kaizen method)
Make change simple and do it often. This way it automatically becomes a habit. - Get immediate feedback
Use a pedometer, smartwatch, or app to immediately see what you achieve. This helps you stay motivated. - Reward yourself in a way that suits you
For example, are you quitting smoking? Put a euro in a piggy bank every day. Rewards help maintain new habits. - Integrate new habits into your daily life
For example, make exercise obvious and easy. Take the bike to the supermarket or do gardening. Do not choose things that are complicated. Do it together with your environment (family, partner, friends). - Link your change to what is really important to you
Change is easier when it contributes to something bigger: your health, your family, or your work. Think about the ‘why’. - Keep it up for at least two months
Habits take time to form. Count on 40-60 days before something becomes automatic. The more complex, the longer it takes. - Keep it realistic: 80-20 rule
You don’t have to be perfect. Make sure 80 percent of your choices are healthy and leave 20 percent room for relaxation and fun. - Be inspired by role models
Idols and influencers can help. Think of Ronaldo who during a press conference at the World Cup swapped cola for water. But also of healthcare providers: ‘The doctor said so’ has (some) effect.
This approach helps you strengthen your lifestyle in an achievable and enjoyable way and maintain changes.
8. Conclusion
Section titled “8. Conclusion”Depression is a complex condition with biological, psychological, and
socio-economic causes, in which metabolic dysfunction plays a still
underexposed role. This article shows that
lifestyle interventions such as healthy nutrition, more exercise, better
sleep, more relaxation, and more meaning can not only improve
metabolic health but can also help with depressive
symptoms. Although existing treatments remain valuable, a
broader approach --- where lifestyle change is an integral part
--- offers new opportunities for recovery and prevention.
Lifestyle adjustments can make a big difference in the long term.
Now it’s up to you: start with a first step, however small, and
experience the impact yourself. Your physical and mental health are
inextricably linked. Work on it and give yourself the
opportunity for a more energetic, resilient life.
Veelgestelde vragen
How does lifestyle help with depression?
A healthy lifestyle improves mood, reduces symptoms of depression, and improves physical health.
Which lifestyle helps with depression?
Healthy nutrition, exercise, good sleep, stress reduction, reducing substance use, and improving sense of meaning.
Which nutrition helps against depression?
A Mediterranean diet (unprocessed food, vegetables, fruit, fish, olive oil, nuts) can significantly reduce depressive symptoms.
Can exercise help against depression?
Yes, exercise such as walking, jogging, and yoga is effective and sometimes even better than antidepressants for mild to moderate depression.
Why is sleep important for depression?
Sleep problems occur in 90 percent of people with depression. An improvement in sleep quality can reduce symptoms.
Does reducing stress help against depression?
Yes, chronic stress increases the risk of depression. Relaxation techniques such as mindfulness help.
How does meaning affect depression?
A strong sense of meaning is associated with fewer depressive symptoms and faster recovery.
Medische Disclaimer: De informatie van Stichting Je Leefstijl Als Medicijn over leefstijl, ziektes en stoornissen mag niet worden opgevat als medisch advies. In geen geval adviseren wij mensen om hun bestaande behandeling te veranderen. We raden mensen met chronische aandoeningen aan om zich over hun behandeling goed door bevoegde medische professionals te laten adviseren.
Medical Disclaimer: The information provided by Stichting Je Leefstijl Als Medicijn regarding lifestyle, diseases, and disorders should not be construed as medical advice. Under no circumstances do we advise people to alter their existing treatment. We recommend that people with chronic conditions seek advice regarding their treatment from qualified medical professionals.